ani:abstracts
Element Information
Model
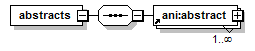
Used By
| Complex Type | ani:headType |
Source
<xs:element name="abstracts"> <xs:complexType> <xs:sequence> <xs:element maxOccurs="unbounded" ref="ani:abstract"/> </xs:sequence> </xs:complexType> </xs:element> |
Sample
|
< head xmlns = "http://www.elsevier.com/xml/ani/ani" xmlns:ce = "http://www.elsevier.com/xml/ani/common" > |
|
[...] |
|
< citation-type code = "ar" /> |
|
Hepatectomy |
|
</ author-keyword> |
|
Laparoscopy |
|
</ author-keyword> |
|
Liver cancer |
|
</ author-keyword> |
|
</ author-keywords> |
|
</ citation-info> |
|
A conceptual technique for laparoscopic right hepatectomy based on facts and oncologic principles: The caudal approach |
|
</ titletext> |
|
</ citation-title> |
|
< author-group> |
|
< ce:initials> |
|
O. |
|
</ ce:initials> |
|
Soubrane O. |
|
</ ce:indexed-name> |
|
< ce:degrees> |
|
MD |
|
</ ce:degrees> |
|
< ce:surname> |
|
Soubrane |
|
</ ce:surname> |
|
Olivier |
|
</ ce:given-name> |
|
< ce:e-address> |
|
olivier.soubrane@sat.aphp.com |
|
</ ce:e-address> |
|
</ author> |
|
< ce:initials> |
|
L. |
|
</ ce:initials> |
|
Schwarz L. |
|
</ ce:indexed-name> |
|
< ce:degrees> |
|
MD |
|
</ ce:degrees> |
|
< ce:surname> |
|
Schwarz |
|
</ ce:surname> |
|
Lilian |
|
</ ce:given-name> |
|
</ author> |
|
< ce:initials> |
|
F. |
|
</ ce:initials> |
|
Cauchy F. |
|
</ ce:indexed-name> |
|
< ce:degrees> |
|
MD |
|
</ ce:degrees> |
|
< ce:surname> |
|
Cauchy |
|
</ ce:surname> |
|
François |
|
</ ce:given-name> |
|
</ author> |
|
< ce:initials> |
|
L.O. |
|
</ ce:initials> |
|
Perotto L.O. |
|
</ ce:indexed-name> |
|
< ce:degrees> |
|
MD |
|
</ ce:degrees> |
|
< ce:surname> |
|
Perotto |
|
</ ce:surname> |
|
Laura Ornella |
|
</ ce:given-name> |
|
</ author> |
|
< ce:initials> |
|
R. |
|
</ ce:initials> |
|
Brustia R. |
|
</ ce:indexed-name> |
|
< ce:degrees> |
|
MD |
|
</ ce:degrees> |
|
< ce:surname> |
|
Brustia |
|
</ ce:surname> |
|
Raffaele |
|
</ ce:given-name> |
|
</ author> |
|
< organization> |
|
Department of Hepatobiliary Surgery and Liver Transplantation, Université Pierre et Marie Curie |
|
</ organization> |
|
< city> |
|
Paris |
|
</ city> |
|
</ affiliation> |
|
</ author-group> |
|
< author-group> |
|
< ce:initials> |
|
D. |
|
</ ce:initials> |
|
Bernard D. |
|
</ ce:indexed-name> |
|
< ce:degrees> |
|
MD |
|
</ ce:degrees> |
|
< ce:surname> |
|
Bernard |
|
</ ce:surname> |
|
Denis |
|
</ ce:given-name> |
|
</ author> |
|
< ce:initials> |
|
O. |
|
</ ce:initials> |
|
Scatton O. |
|
</ ce:indexed-name> |
|
< ce:degrees> |
|
MD Ph.D. |
|
</ ce:degrees> |
|
< ce:surname> |
|
Scatton |
|
</ ce:surname> |
|
Olivier |
|
</ ce:given-name> |
|
</ author> |
|
< organization> |
|
Department of Anesthesiology, Hôpital Saint Antoine, Assistance Publique-Hôpitaux de Paris |
|
</ organization> |
|
< city> |
|
Paris |
|
</ city> |
|
</ affiliation> |
|
</ author-group> |
|
< author-group> |
|
< ce:initials> |
|
O. |
|
</ ce:initials> |
|
Soubrane O. |
|
</ ce:indexed-name> |
|
< ce:degrees> |
|
MD |
|
</ ce:degrees> |
|
< ce:surname> |
|
Soubrane |
|
</ ce:surname> |
|
Olivier |
|
</ ce:given-name> |
|
< ce:e-address> |
|
olivier.soubrane@sat.aphp.com |
|
</ ce:e-address> |
|
</ author> |
|
< organization> |
|
Department of Hepatobiliary Surgery and Liver Transplantation, Hôpital Saint Antoine |
|
</ organization> |
|
< address-part> |
|
184, rue du Faubourg Saint Antoine |
|
</ address-part> |
|
< city> |
|
Paris |
|
</ city> |
|
< postal-code> |
|
75012 |
|
</ postal-code> |
|
</ affiliation> |
|
</ author-group> |
|
< person> |
|
< ce:initials> |
|
O. |
|
</ ce:initials> |
|
Soubrane O. |
|
</ ce:indexed-name> |
|
< ce:degrees> |
|
MD |
|
</ ce:degrees> |
|
< ce:surname> |
|
Soubrane |
|
</ ce:surname> |
|
Olivier |
|
</ ce:given-name> |
|
</ person> |
|
< organization> |
|
Department of Hepatobiliary Surgery and Liver Transplantation, Hôpital Saint Antoine |
|
</ organization> |
|
< address-part> |
|
184, rue du Faubourg Saint Antoine |
|
</ address-part> |
|
< city> |
|
Paris |
|
</ city> |
|
< postal-code> |
|
75012 |
|
</ postal-code> |
|
</ affiliation> |
|
</ correspondence> |
|
< grant> |
|
NIH |
|
</ grant-acronym> |
|
< grant-agency> |
|
Wellcome Trust |
|
</ grant-agency> |
|
</ grant> |
|
< grant> |
|
< grant-agency> |
|
Wellcome Trust |
|
</ grant-agency> |
|
</ grant> |
|
< grant> |
|
HHMI |
|
</ grant-acronym> |
|
< grant-agency> |
|
Wellcome Trust |
|
</ grant-agency> |
|
</ grant> |
|
< grant-text> |
|
The authors declare no conflict of interest, funding, grant equipment, and drugs. The authors declare not having received funding for this work from any of the following organizations: National Institutes of Health (NIH); Wellcome Trust; Howard Hughes Medical Institute (HHMI); or other(s). O.S. and O.Sc. designed the study. L.S., O.P., F.C. collected the data. All authors participated in interpreting the data, drafting the article, and revising it critically for intellectual content and gave their final approval of the version submitted for publication. All authors have seen, approved, and are fully conversant with the contents of the manuscript. All authors are responsible for the accuracy of the manuscript, including the statistical calculations. |
|
</ grant-text> |
|
</ grantlist> |
|
< abstracts> |
|
Copyright © 2014 Wolters Kluwer Health, Inc. All rights reserved. |
|
< ce:para> |
|
Objective: To evaluate a new conceptual technique of laparoscopic right hepatectomy Background: Despite significant improvements in surgical care in the last decades, morbidity is still high after major hepatectomy. Blood loss and transfusions are known to significantly increase the risk of postoperative complications and cancer recurrence after liver resection. A laparoscopic approach may improve perioperative outcomes in these cases, but data in literature are limited and the surgical technique is not yet standardized. Methods: A new conceptual technique of right hepatectomy was designed using evidence-based facts and oncologic rules: laparoscopy with pneumoperitoneum, low central venous pressure, intermittent pedicle clamping, anterior approach without mobilization, and parenchymal section with ultrasonic dissector. Thirty patients were prospectively enrolled between October 2011 and September 2013. Primary endpoint was intraoperative blood loss. Results: Eighty percent of patients underwent surgery for malignant disease and cirrhosis was present in 11 patients. Benign lesions accounted for 13% of indications, whereas living liver donation was performed in 2 cases. Median blood loss was 100 mL (50-700) and transfusion rate was 7%. Five patients (16.6%) required conversion to laparotomy, including 2 using hybrid technique. The median operative time was 360 minutes (210-510). R0 resection rate was 87% (21/24). Postoperative morbidity rate was 23% (7/30) with 8 complications including 6 Clavien III-IV. No respiratory complication occurred. The median hospital stay was 8 days. No patient died. Conclusions: This study showed that several evidence-based facts could be combined to define a new conceptual technique of laparoscopic right hepatectomy allowing for low blood loss and morbidity. |
|
</ ce:para> |
|
</ abstract> |
|
</ abstracts> |
|
< sourcetitle> |
|
Annals of Surgery |
|
</ sourcetitle> |
|
Ann. Surg. |
|
Annals of Surgery |
|
15281140 |